Measure Immune Response to Predict Outcomes
By Kevin Flanagan, PhD
Oncologists and cancer patients alike carefully track tumor status. The tumor is growing. The tumor is shrinking. The tumor has spread. The tumor is stable. There are new tumors. There are fewer tumors. Tumor size and number is visualized with various imaging techniques such as x-rays, ultrasounds, and MRIs. A number of biomarkers are also used to track cancer status, such as measuring serum CA 15-3 to monitor breast cancer. While it is easy to understand the importance of monitoring a patient’s tumor(s), often it is also important to measure immune response.
This is true for patients receiving traditional therapies like chemotherapy or radiation, as well as for patients receiving immunotherapies such as checkpoint inhibitors or CAR-T cell therapies. The immune system plays a critical role in tumor development and progression, and its response to cancer and cancer therapies can be helpful in assessing prognosis and predicting the effectiveness of therapies even before the tumor itself responds. Likewise, many cancer treatments weaken the immune system, leaving the patient susceptible to infection and disease. Immunotherapies work by modulating the immune system, and sometimes they drive overactive immune responses that can be life threatening to the patient. Measuring immune response and identifying these conditions early can save patients time, money, and even their lives.
Despite the need for accurate measurements of immune response, it is often difficult to do in a meaningful way. Lymphocytes and myeloid cells are the two major classes of immune cells. Measuring tumor infiltrating lymphocytes (TILs) is predictive of outcome for many indication/therapy paradigms. However, a simple count of TILs does not account for the actual makeup of immune cell types, the activation status of the TILs, or the influence of non-lymphoid cells such as Myeloid-Derived Suppressor Cells (MDSCs), which inhibit the immune response. In some contexts, measuring subsets of TILs is more predictive than looking at the total lymphocyte infiltration. Therefore, it is important to monitor specific immune cell populations, rather than the total immune cell or TIL population.
Myriad immune cell types have distinct functions in the tumor microenvironment. Immune cells include T cells, B cells, macrophages, Natural Killer (NK) cells, and many more. Each of these cell types can be subtyped into smaller classes. As an example, T cells have two main subcategories, CD4-positive and CD8-positive. Within just one of those subcategories are tens of subtypes and activation states. Single-cell RNA-sequencing is further increasing the number of putative subtypes. Considering T cells are just one of many immune cell types, the diversity of immune cells becomes clear.
Likewise, the immune response to cancer is complex. Many of these immune cell subtypes have either pro- or anti-tumorigenic effects, often depending on context. For example, CD8-positive T cells are generally anti-tumorigenic, while CD4-positive Regulatory T cells are typically pro-tumorigenic. Further, immune cell activity is variable and affected by signaling from tumor and immune cells, the degree and duration of antigen exposure, and other factors. Ultimately, the effect of the immune response is dependent on the interplay between immune cells, tumor cells, stromal cells, and therapeutic intervention. Importantly, clinical monitoring and measuring immune response requires distilling the relevant aspects of this complex interplay down to clinically useful insights.
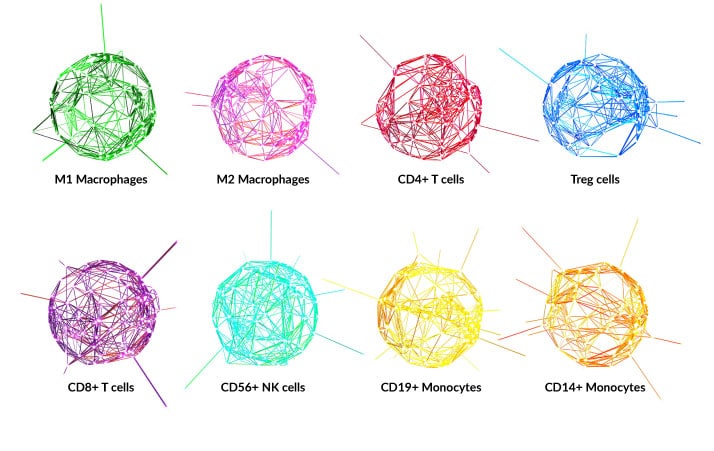
While it is not yet wholly apparent which details might be important for informing clinical decisions, it is clear that robust, comprehensive methods are needed to capture the diversity of the tumor immune microenvironment. H&E staining has traditionally been used to measure TILs. Additionally, immunohistochemistry (IHC) is used to identify many immune cell markers. However, the ability of these histopathological methods to comprehensively measure immune response is limited by tissue quantity, antibody and staining variability, and a lack of protein markers to define many immune cell types. Newer techniques, including multiplexed IHC and tissue microarrays, are able to overcome some of these limitations. For fresh tissues and blood, flow cytometry can readily identify many cell subtypes and activation states. Unfortunately, most relevant patient samples are formalin-fixed paraffin-embedded (FFPE), not fresh. For FFPE tissue, new technologies like Cofactor’s ImmunoPrismᵀᴹ use RNA-based Health Expression Models to estimate immune cell content in a more comprehensive way than traditional IHC. ImmunoPrismᵀᴹ estimates the abundance of eight immune cell types, measures expression of immune-relevant genes such as PD-1 and CTLA-4, and uses Predictive Immune Modeling to classify patients based on multidimensional biomarkers. Moving forward, technologies like ImmunoPrismᵀᴹ will be used to probe the importance of various immune contexts, monitor disease progression, and predict therapeutic response.