Immune Modeling
By Rachel Wellinghoff
Disease is complex. This statement seems so evident, but behind it lies an entirely new way to approach oncology. Previous methods have targeted single analytes, prescribing a one-treatment meets all outlook to every patient. As we know, due to disease heterogeneity, these standard treatments are only effective in a subset of the patient population.¹ A better understanding of why some patients see success with certain treatments can help match candidates to more effective therapies. One way to do this is through utilization of the predictive power of RNA and predictive immune modeling. Next-generation sequencing (NGS) has revealed a mutational diversity in tumors that emphasizes the need for personalized care that exploits the unique profile of each tumor.²
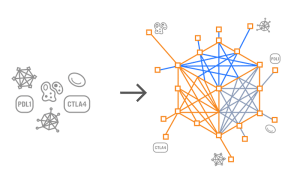
Understanding immune response is of paramount importance for oncology. Immunotherapies harness a patients’ own immune system to fight cancer, and can include such treatments as monoclonal antibodies, checkpoint inhibitors, cytokines, vaccines, adoptive cell transfer and companion diagnostics.¹ Tumor development and progression is heavily influenced by the immune system; monitoring of the immune system can help assess effectiveness of treatments, often even before the tumor itself responds. For this reason, looking at disease from a single viewpoint (analyte) is incredibly limited in scope and clearly doesn’t display the entire picture; thus, a single analyte is restricted in its ability to help predict and understand disease. Although this attempt to link a single molecular entity to tumor behavior does generate statistically significant predictors, the clinical utility of these predictive strengths is suboptimal.³ A novel, multidimensional approach overcomes these deficiencies and has “the potential to meaningfully guide the selection of therapeutic strategies for individual patients while elucidating molecular mechanisms driving disease progression,” while also revealing agents and pathways playing prominent roles in tumor development.³
Disease is complex. To truly adopt this stance, to embrace it, and in turn a better way in which to treat cancer, means looking at potential treatments as complex. Recently, it has become evident that no two patients’ cancers are the same and, therefore, variable responses to standard treatments such as chemotherapy and radiation are expected. The traditional model for cancer therapy is too simplistic; a new model, one based on the power of personalized medicine, aims to thwart this failed “one size fits all” approach to cancer therapies.¹ Treatments will differ based on the individual, the cancer and a predicted/observed response. To do this, medical care will be based on the microenvironment of the cancer, as well as on the body’s response to this invader; it will take into account and use as a target a multidimensional analyte model approach to a cure. It will respond to both the cancer and the patient.
Big data generated by NGS is only useful if the results can be interpreted and applied to patients in the field of oncology. Health Expression Models, created by Cofactor Genomics, represent multiple facets of biology by looking at the dynamic expression levels that can be influenced by the state of a disease, environment, therapies, etc. This detection and documentation of immune cells opens the door to a more sophisticated approach to immune profiling. Building Health Expression Models for key immune cell types that have shown promise – both independently and in an interconnected fashion – in predictive therapy response is the first step to better understand disease and anticipate treatment reaction. It is this use of Predictive Immune Modeling stemming from multidimensional biomarkers, based on Health Expression Models, that captures the full picture of the immune response at the tumor within the context of clinical data in a robust, multidimensional model. It is clear that integrating a personalized approach into cancer research and subsequent treatments will result in major improvements in fighting cancer, countering its’ native complexity and interpatient variability.¹ Correlating the immune details elucidated by Health Expression Models alongside tumor monitoring in a clinically meaningful manner has the potential to transform cancer care on a personal level.
Disease is complex, and so are the individuals who we, as a global society, treat. It only makes sense that our perspective on medical care and effective therapies is equally complex.
REFERENCES
- Krzyszczyk P, Acevedo A, Davidoff E, Timmins L, et al. (2018). The growing role of precision and personalized medicine for cancer treatment. Technology (Singap World Sci) 6(3-4): 79-100.
- Martin SD, Coukos G, Holt RA, Nelson BH. (2015). Targeting the undruggable: immunotherapy meets personalized oncology in the genomic era. Ann Oncol 26(12): 2367-2374.
- Mariana M, He S, McHugh M, Andreoli M, Pandya D, et al. (2014). Integrated multidimensional analysis is required for accurate prognostic biomarkers in colorectal cancer. PLoS ONE 9(7): e101065.
Cofactor offers products both for Research Use Only (not to be used as a diagnostic assay) and within our CAP-certified laboratory. Please contact us to discuss which option is right for your application.